
During my first EMT course, our instructor outlined the phases of a patient encounter: scene safety, general impression, primary assessment, secondary assessment, and reassessment.
If you’ve ever done the psycho-motor skills exam, this probably sounds familiar. After working on an ambulance, I quickly learned this organized approach was somewhat academic.
by J. Bridger, contributing author
Things don’t happen in real life the way they do in textbooks. Real life is messy. Not all patients want you there, not all calls are exciting, not all calls warrant a head-to-toe trauma scan. That being said, I can appreciate the idea behind it. You may have heard the saying, “You don’t rise to the occasion, you fall to your level of training.” Drilling this into your brain gives you something to fall back on when your adrenaline is flowing, and you aren’t sure what to do next. With experience, you can tailor it to fit your needs.
You can argue that the primary assessment is the most crucial part of a patient encounter (not counting responder safety!). It is easily taught to any motivated responder, whatever their level of training may be. You don’t need to be a nationally registered critical care paramedic to apply direct pressure to a bleed. I’d like to focus more on what needs to happen than how. The how depends on your level of education, training, certification, and tools at hand. The goal of a primary assessment is simple: to find and treat life threats. Let’s break it down step by step.
Again, the primary assessment’s goal is to FIND and TREAT life threats. Let me be extremely clear: This means you are not applying a loose dry bandage or Water-Jel to your patient’s burned forearm; you are not splinting that tib-fib fracture; you are not applying a protective eye shield to that wounded orbit. These things will come later. You are only searching for things that will kill your patient and fixing them.
ABC – Airway, Breathing, and Circulation
In EMT school, we learned the primary assessment as “Your ABCs.” Airway, breathing, and circulation. ABC is great, but I prefer MARCH, which I learned in TCCC (Tactical Combat Casualty Care). MARCH rearranges the ABCs, putting the thing that will kill your patient first at the top of the list – Massive hemorrhage. Hemorrhage is just a spelling bee word for bleeding. Somewhere in my EMS training we learned CAB, which places circulation at the front of the ABCs. They reported this change only delays airway assessment by 17 seconds; I have no idea how that number was found.
What Does MARCH Stand For?
MARCH is better than ABC It stands for:
- M = Massive hemorrhage
- A = Airway
- R = Respirations
- C = Circulation
- H = Hypothermia & Head injury

You can see MARCH begins with bleeding, which is covered in C of ABCs. Then it’s basically ABC, with respirations taking the place of B. They add on hypothermia and head injury at the end. Let’s break each step down, then we will discuss treatment.
Also: Please don’t neglect responder safety. Have nitrile gloves, keep your head on a swivel, and work in pairs whenever possible. Don’t get tunnel vision. Don’t let anyone between you and the way out. Consider establishing a codeword with your partner that means “I don’t feel safe, something is wrong, let’s get out of here.”
MARCH Assessment
M = Massive Hemorrhage Assessment
A bad bleed will kill your patient quickly. TCCC references data that says approximately 2/3 of preventable battlefield deaths are attributed to extremity hemorrhage. A battlefield may be a lot different from our typical work environment, but with the mass shootings we are experiencing, I feel it’s important to incorporate this into our training.
The way we assess massive hemorrhage is by doing a blood sweep. You may elect to skip this step if the situation calls for it. For example, you are responding and find the call to be non-traumatic, and it’s obvious the patient is not bleeding.
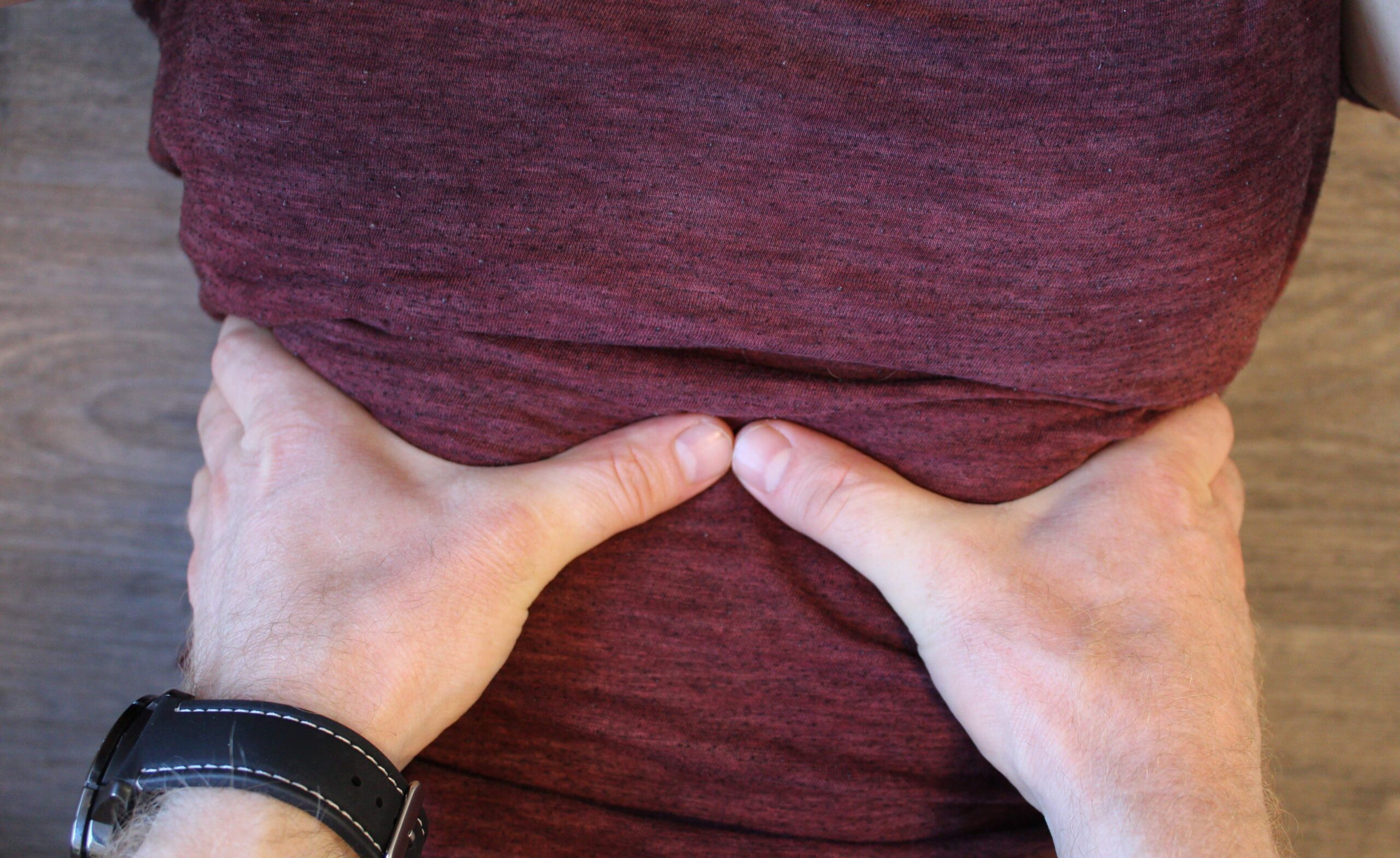
To do a blood sweep, you simply sweep your gloved hands behind the patient’s head and look at them. Any blood? No? Go on. Yes? Consider if it is life threatening and requires immediate treatment. Continue until you’ve checked the neck, arms, torso, abdomen, legs, back, the entire body. A life-threatening bleed may be obvious just by looking at the patient. However, once you’ve treated it, you should still do a blood sweep to make sure you haven’t missed anything. Keep in mind, on porous dirt, a lot of blood doesn’t look that impressive. On a tile floor however, a little blood can cover a large area. Black nitrile gloves look cool, but blood doesn’t show up well on them, especially in low light. I prefer blue or orange gloves for this reason. A blood sweep is also a great opportunity to feel for weapons, if you are so inclined.
A = Airway Assessment
The goal is to maintain an open airway. No airway means your patient can’t breathe, and will die. If your patient is talking without difficulty, then you can conclude the airway is patent (adequate). If your patient is unconscious, it may not be so obvious. Can you feel or hear air moving from their mouth or nose? If you hear gurgling on exhalation, there may be blood, vomit, or other fluid in the airway. A high-pitched whistling noise upon inspiration (called stridor) may indicate an upper airway obstruction. “Snoring” respirations may indicate the tongue is occluding or blocking the airway. If you see a blue tint to the lips or face (cyanosis) you should suspect the patient is not moving air.
R = Respirations Assessment
To assess respirations, you should expose the chest. When you breathe, the diaphragm moves down and your chest expands. The increase in volume decreases pressure in your lungs and draws air in. Simply put, you are watching for symmetrical chest rise on both sides. There should be adequate depth, normal rate, and normal rhythm.
For an adult, a normal rate is 12-20 breaths per minute (1 every 3-5 seconds). Keep in mind this may change for many reasons, as a normal response to an event or indicating something worse. Place your hands on the patient’s ribs with your thumbs touching. If your patient is able, instruct them to take a large breath. Both sides of the chest should expand equally, moving both of your thumbs away from each other. The condition we are trying to rule out in this part of the assessment is a pneumothorax. A pneumothorax can be primary (due to injury, or spontaneously) or secondary (due to a disease process).
Your lungs are covered by a continuous visceral (against the organs) and parietal (against the chest wall) membrane, called the pleura. When air enters the potential space between them, it can get trapped. Every breath adds more pressure the lung must expand against. If untreated, the pressure can push against the mediastinum (the area between the lungs containing the great vessels, heart, and portions of the trachea) reducing venous return to the heart and cardiac output, leading to obstructive shock.
This is called a tension pneumothorax. A pneumothorax can cause tracheal deviation (away from the affected side), engorged jugular veins (called JVD, or jugular vein distention), absent or decreased breath sounds over the affect area, chest pain, and dyspnea (an uncomfortable awareness of difficulty breathing). It may even be totally asymptomatic. Just because there is no penetrating trauma to the chest does not mean a pneumothorax is not present.
Another condition to be aware of is flail chest. When rib segments break in two or more places, they can move paradoxically (think “opposite”) with the chest. This impairs ventilation. If you see it, you won’t forget what it looks like!
C = Circulation Assessment

Assessing circulation helps determine if shock is present. Shock is a state of hypoperfusion; i.e. low oxygenation to the tissues. Untreated, shock will result in death. A patient may be experiencing compensated, decompensated, or irreversible shock. Shock is an interesting and lengthy topic.
For our purposes, I recommend you trust that shock kills, and it is easier to prevent than treat. To assess for adequate circulation, you should note the mental status of the patient, if conscious. If the patient can speak, they may say they feel cold, thirsty, or a “sense of impending doom.” Assess the skin temperature and color. Pale, cool skin suggests inadequate circulation. Feel for a radial pulse. An absent radial pulse suggests low blood pressure. A good rule of thumb is altered mental status and no radial pulse suggests shock is present. The patient requires aggressive treatment.
Some sources teach capillary refill for everyone, others say it is unreliable in anyone over 8 years old. You should be aware of this technique regardless. To do this, blanch a finger or toe nail by squeezing it, and release. The color should return in less than 3 seconds. If it does not, you should assume a circulation problem.
H = Hypothermia / Head Injury Assessment
It is important to keep patients warm. Hypothermia interferes with the blood’s ability to coagulate, making patients more susceptible to bleeding. Shivering and pale or blue skin (lips and nail beds) are clues to look for in a cold patient. Even if the air temperature is not what we would think of as cold, a hypovolemic or wet patient may be losing heat. Keep in mind a patient on the ground or a cold floor may be losing heat rapidly.
You should visually inspect and palpate (feel) the skull for any injuries. Altered mental status, vomiting, posturing, erratic breathing, or unequal/sluggish pupils may be signs of a head injury. One of the dangerous things about head injuries is intracranial pressure caused by bleeding or swelling of your think-meat. We can displace a little blood, and we can displace a little cerebrospinal fluid (CSF), but displacing brain can have a very poor outcome.
Now that you have a little background, let’s discuss treatment in each of these categories.
MARCH Treatment
M = Massive Hemorrhage Treatment
If you find a life-threatening bleed, treatment depends on location of the injury. If the injury is on an extremity, applying a tourniquet (TQ) high and tight (Like a giraffe’s butthole) is the life saving intervention. There are a lot of myths about TQ’s, and they are just that: Myths.
Consider this: In a 2008 article called “The Safety of Tourniquet Use” (by Kragh) in the Journal of Trauma, 232 patients had tourniquets on 309 limbs. No limbs were lost due to tourniquet use, and only 3% developed transient nerve palsy.

Mil-spec tourniquets can be bought online, but before applying a TQ, be sure no unintended part of your patient’s anatomy will be caught in it. Make sure nothing in their pockets is in the way of the TQ. If one TQ doesn’t stop the bleeding, add another.
Every time you move your patient, check that the TQ has not come loose. If the bleed is due to a junctional wound (eg: at the neck and shoulder, or the hip flexor-inguinal area) where you cannot place a TQ, you must apply direct pressure. Purpose-made junctional bleed devices exist, but I find them bulky. If the bleed is in the inguinal/hip flexor area, you can occlude the artery by taking a knee and placing it above the wound and putting your weight on it, occluding or obstructing the iliac artery (which becomes the femoral artery).
Direct pressure with a standard trauma dressing should stop bleeding in 10 minutes. If you use a hemostatic agent (aids in coagulation) like Quikclot or Celox, that time shrinks to 3 minutes. Ten minutes is an eternity when you have other things you need to do. Get a z-fold hemostatic agent, pack it in the wound and press like the person’s life depends on it! For abdominal wounds, you do not want to pack gauze. You can pack all day, and you’ll just give them a gauze baby. Use a large occlusive trauma dressing with direct pressure.
A = Airway Treatment
You must open and maintain your patient’s airway! If you suspect fluid in the airway, the patient should be rolled onto their side in the recovery position. If they are unconscious and suction is available, use it. If you hear snoring respirations, a head-tilt-chin-lift should open the airway. If you suspect spinal trauma, use a jaw-thrust maneuver. As far as I know, you don’t need any certification to roll a patient over or use manual maneuvers to open an airway.
If you are certified and can use an oropharyngeal airway (OPA) or nasopharyngeal airway (NPA), those are good adjuncts. I think OPAs go in quicker, but I like NPAs because you can use them with an intact gag reflex, provided you do not suspect head injury. There are many other advanced airways that I won’t discuss here, in the interest of brevity. If advanced airways are in your scope of practice, there isn’t anything I can teach you in a short article that you don’t already know. The goal is to establish a patent airway for your patient.
R = Respirations Treatment
If your patient has an open chest wound, you should quickly apply a chest seal (Don’t forget to check the patient’s back!). There are many kinds of chest seals available, but I would recommend using one that is vented. If you do not use a vented seal, and your patient begins to experience difficulty breathing, you should relieve pressure by peeling up one corner of the seal and allowing pressure to escape. If you suspect a closed pneumothorax, and you have the training and equipment, you may need to perform a needle decompression. I won’t go into detail about this. Locating the anatomical landmarks can be difficult, and if you aren’t trained and certified, you really open yourself up to legal trouble. I will save the details for a future article! To treat a flail chest, you should use a bulky dressing to stabilize the affected segment.
C = Circulation Treatment
Even if your findings do not suggest shock, you may want to treat for shock to prevent it. Keep your patient warm. Elevate their legs. Administer oxygen if possible. If you have IV equipment available, only give enough fluids (warmed if possible) to maintain a radial pulse.
H = Hypothermia / Head Injury Treatment

This one is easy. Keep them warm. (You should already be doing this no matter what!) Keep the patient off the cold ground, give them a blanket. Purpose made air activated heat blankets (like hand warmers) exist and are wonderful for this. Hypothermia, like shock, is better prevented than treated. Head injuries are difficult to manage. Manually stabilizing the cervical spine or using a c-collar may be all you are able to do. Ensure adequate oxygenation. The patient needs to be transferred to a higher level of care.
Importance of Reassessment
My EMT books would say “reassess critical patients every 5 minutes, and non-critical patients every 15 minutes.” Reassess their vitals, interventions you have performed, and your primary assessment. I would continually reassess your patient and be alert to any changes in their condition.
The only way to get good at this is to practice.
Make sure you know what normal respirations look, feel, and sound like. Make sure you can find a pulse. Go over it in your head in the shower, or on your way to work. Memorize MARCH until it is second nature. At the very least, I hope you do not feel clueless or helpless if you should be first on scene with a patient. If nothing else can be done, consider this: good medicine cures sometimes, relieves often, and comforts always. If someone is experiencing the worst day of their life and you don’t have the knowledge or tools to do anything, comfort and reassurance may be the best thing you can provide.
Disclaimer: There is more than one way to manage a patient encounter! This article is not a substitute for education and training. Always consult local protocols.
Related J Bridger article: The Individual Trauma Kit / IFAK
About the author: J Bridger hails from the Southwest US, where he is currently attending a Physician Assistant (PA) program, holds Advanced EMT, Advanced Cardiac Life Support, Pediatric Advanced Life Support, Tactical Combat Casualty Care, and Tactical Emergency Casualty Care certifications, is a captain on a local FD, and holds private pilot and sUAS licenses, Open Water SCUBA certification, and Extra Class Amateur Radio Operator License.
2 comments
while i agree 100% of the story there are those of us like myself that have seen TO MUCH of death and mayhem as i have PTSD from a NUMBER of bad things that happened to me there are those that CAN do this kind of work then there are other like myself that if i found myself in this kinda situation i would be in a flash back in seconds me i just couldnt handle it
Wow… I’ve had my share of civilian-based (though highly effective) TCCC training and I must say, some of the nuances you intro’d are quite helpful (BloodScan simultaneously checks for weaps, Shock easier to avoid than treat, and some VERY CLEAR delineations of Wound protocols that makes things more clear and is veryVeryVERY clear… SO THANK YOU FOR THAT!
One quickie thought on the ‘protect patient from the ground’ ALSO applies to it being too hot and increasing body temp and/or scalding the skin (more opp for infection). Here in AZ the dogs can’t be walked during extreme Summer (June – Aug/Sep) daylight/early evening hours until the concrete cools down enough for their paws (or they wear those booties).
Good stuff, man, and first time here; I’ll be back (thanks again to Greg Ellifritz wbo’s intro’d us to alotta really shcmart folks out there).